Management of Prolapse
Patients complain of feeling a lump in between the legs or a dragging sensation at the end of the day may have prolapse.
It can be very embarrassing for the patients to discuss, but it is good to know that many women suffer from this condition, and it can be managed leading to a better quality of life.
Dr Joshi after detail examination will offer surgical or non-surgical management for prolapse.
Simplistically speaking, the organs within a woman’s pelvis (uterus, bladder and rectum) are normally held in place by ligaments and muscles known as the pelvic floor. Prolapse occurs If these support structures are weakened by overstretching and the pelvic organs can bulge (prolapse) from their natural position into the vagina. Sometimes a prolapse may be large enough to protrude outside the vagina.
Key points
- Prolapse is very common. Mild prolapse often causes no symptoms and treatment is not always necessary.
- Prolapse can affect quality of life by causing symptoms such as discomfort or a feeling of heaviness. It can cause bladder and bowel problems, and sexual activity may also be affected.
- Prolapse can be reduced with various lifestyle interventions including stopping smoking, weight loss, exercise and avoiding constipation, as well as avoidance of activities that may make your prolapse worse such as heavy lifting.
- Treatment options to support your prolapse include physiotherapy, pessaries and surgery.
- How severe your symptoms are and whether you choose to have surgery will depend on how your prolapse affects your daily life. Not everyone with prolapse needs surgery.
- Surgery for prolapse aims to support the pelvic organs and to help ease your symptoms.
Half of women over 50 will have some symptoms of pelvic organ prolapse and one in ten will have had surgery for prolapse.
- Being pregnant and giving birth are the most common causes of weakening of the pelvic floor. Performing pelvic floor exercises is very important after childbirth but may not prevent prolapse from occurring.
- Prolapse is more common as you get older, particularly after menopause.
- Being overweight can weaken the pelvic floor.
- Constipation, persistent coughing or prolonged heavy lifting can cause a strain to the pelvic floor and can cause pelvic organ prolapse.
- Following hysterectomy, the top of the vagina is supported by ligaments and muscles. If these supports weaken, a vault prolapse may occur (see below).
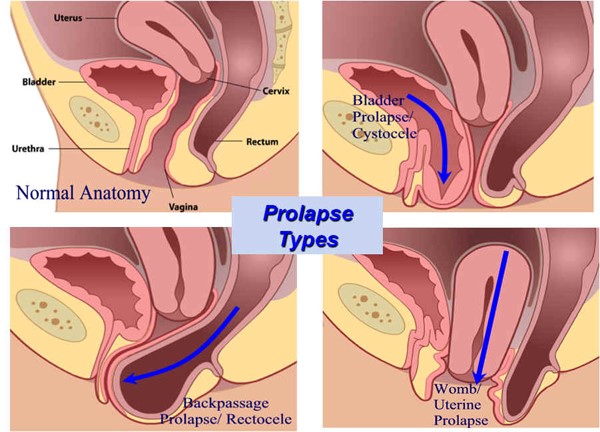
There are different types of prolapse depending on which organ is bulging into the vagina. The uterus, bladder, or rectum may be involved. It is common to have more than one type of prolapse at the same time.
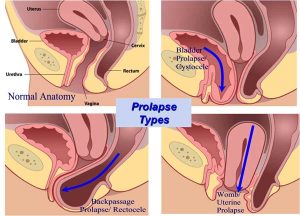
The most common types of prolapse are:
- Anterior wall prolapse (cystocele) – when the bladder bulges into the front wall of the vagina.
- Posterior wall prolapse (rectocele) – when the rectum bulges into the back wall of the vagina.
- Uterine prolapse – when the uterus hangs down into the vagina. Eventually the uterus may protrude outside the body.
- Vault prolapse – after a hysterectomy has been performed, the top (or vault) of the vagina may bulge down.
Your symptoms will depend on the type and severity of your prolapse.
- The most common symptom is the sensation of a lump ‘coming down’. You may also have had backache, heaviness or a dragging discomfort inside your vagina.
- You may be able to feel or see a lump or bulge. You should see your doctor if this is the case because the prolapse may become sore, ulcerated or infected.
- If your bladder has prolapsed into the vagina, you may:
- experience the need to pass urine more frequently
- have difficulty in passing urine or a sensation that your bladder is not emptying properly
- leak urine when coughing, laughing or lifting heavy objects
- Have frequent urinary tract infections (cystitis).
- Sex may be uncomfortable and you may also experience a lack of sensation during intercourse.
A prolapse is diagnosed by performing a vaginal examination. Your doctor will usually insert a speculum (a plastic or metal instrument used to separate the walls of the vagina to show or reach the cervix) into the vagina to see exactly which organ(s) are prolapsing.
The following may ease your symptoms and stop your prolapse from becoming worse:
- Lifestyle changes
- Losing weight if you are overweight
- Managing a chronic cough if you have one; stopping smoking will help
- Avoiding constipation
- Avoiding heavy lifting
- Avoiding physical activity such as trampolining or high-impact exercise.
- Pelvic floor exercises may help to strengthen your pelvic floor muscles.
- Vaginal hormone treatment (estrogen)
If you have a mild prolapse and you have gone through the menopause; your doctor may recommend vaginal tablets or cream.
Your options for treatment will depend on the type of prolapse you have, how severe it is and your individual circumstances. Treatment options include the following.
Pessary
Surgery
There are many different operations that can be performed to treat prolapse.
Possible operations include:
Vaginal prolapse repair- may include repair of the posterior or anterior vaginal wall A procedure called posterior or anterior colporrhaphy is used in the repairs.
Uterine prolapse repair –Sacrohysteropexy- surgery to suspend the uterus is a recently developed option, which uses the sutures to support the uterus in place.
Hysterectomy is an effective way to resolve uterine prolapse. It may need to be combined with one or more of the other surgical procedure is for repair of the vaginal walls, if they are prolapsing.
Vaginal vault (top of vagina) prolapse repair – Sacrospinous ligament fixation – the surgery to support the top of the vagina can also be performed. Alternatively Sacrocolpopexy or vaginal mesh procedures for the vault support can also be performed; however they come with high risk of complications.
- A pelvic floor repair if you have prolapse of the anterior or posterior walls of the vagina
(Cystocele or rectocele); this is where the walls of your vagina are tightened up to support the pelvic organs.
- Operations that aim to lift up and attach your uterus or vagina to a bone towards the bottom of your spine or a ligament within your pelvis (sacrocolpopexy or sacrospinous fixation)
- A vaginal hysterectomy (removal of the uterus) is sometimes performed for uterine prolapse.
All the surgical procedures come with their own risks and some risks can be life-threatening.
For surgical prolapse repair, the failure rate is 5 to 10 woman out of hundred. Out of hundred, 30 woman may require another operation to treat the recurrence of prolapse.
Up to 5 woman out of hundred may experience painful intercourse or develop stress incontinence and 15 out of hundred women may experience difficulty passing urine.
Between 10 to 20 women may experience complications of mesh.
Two patients out of thousand may experience injury to the bladder and other urinary organs requiring further surgical repair.
RANZCOG Patient Information Guides
https://www.racgp.org.au/afp/2015/july/pelvic-organ-prolapse-%E2%80%93-a-review/
https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/diagnosis-treatment/drc-20353464
https://www.acog.org/Patients/Patient-Education-Videos/Pelvic-Organ-Prolapse (Very good Videos)

